In coronavirus war, hang on, help is on the way with COVID-19 vaccine: Anthony Fauci Q&A
Anthony Fauci | 19 November 2020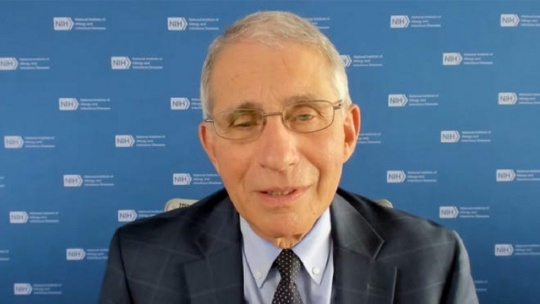
Dr. Anthony Fauci: When the COVID-19 vaccine gets approved by the FDA, I would take the vaccine and I would recommend that my family take the vaccine.
With U.S. coronavirus deaths passing 250,000 and at least two effective vaccines on the horizon, the USA TODAY Editorial Board spoke Wednesday with Dr. Anthony Fauci, the nation’s leading authority on infectious diseases. Fauci, who turns 80 next month, has been director of the National Institute of Allergy and Infectious Diseases since 1984. Questions and answers have been edited for length, clarity and flow:
Q: At what point did you realize that this novel coronavirus was not another drill, that it was your worst nightmare coming to pass?
A: It was really a gradual thing that went from an uneasiness to a real concern to ‘oh, my goodness, it's here.’ When I saw what the Chinese were doing, starting to build a lot of hospitals like overnight, (we knew) there's something really bad going on there. At the end of January we had our first case (in the United States). Very soon thereafter, it became clear that there was community spread. That's when I knew we were in for some serious trouble, particularly with what was going on in China. And then when Italy exploded, it just nailed it down that it's going to be really a problem.
Q: We're in an excruciating time where the virus is surging throughout the country even as apparently safe and effective vaccines are on the horizon. What's the most important thing for people to do between now and when the cavalry arrives?
A: The cavalry is on its way. It's not here yet, but it's going to come. We have an even better than expected efficacy signal on two vaccines. We're likely to already start having distribution of doses, hopefully by the end of December but certainly no later than at the beginning of January. If we can hang on and implement the public health measures, help is really on the way.
Q. What about COVID fatigue and denialism?
A. Even in some of the states where they're getting really hit badly, we're hearing people even denying there's a problem as their hospitals are getting filled. I think that's a spillover of a combination of fatigue for people who are trying (to stay safe) and denial for people who always think that everything is fake news. It really becomes an unprecedented public health challenge.
Q. Do we need a lockdown?
A. You don't need to shut everything down. You just have to look at where you're having the spread and make sure you put a bit of a clamp on that without shutting down every shop and every small business. You don't need to do that. I find it so frustrating that when I (talk about) the five measures — uniform wearing of masks; physical distance; avoiding congregate settings, particularly indoors; trying to do things, to the extent possible that weather allows, outdoors more than indoors; and washing hands — people sometimes interpret that as shutting down. That's not shutting down. That's implementing public health measures at the same time as you keep things open.
Q. Why is the virus spreading so quickly?
A. Many of the infections today are in innocent family and friend dinner gatherings at home because of the almost intuitive instinct that, when you're with family and friends and nobody appears to be physically ill, it's OK to congregate 10 or 12 people for drinks or for a meal or what have you. But it's indoors because the weather is cold. That's where we're seeing these types of outbreaks. As we get into the colder weather, we should really think twice about these kinds of dinner parties.
Q. Like Thanksgiving dinner?
A. With Thanksgiving next week, people have to reevaluate and take a risk-benefit assessment for their own individual family unit as to whether they want to have a big family gathering now, particularly as cases are surging in almost every single part of the country.
Q: Is it safe to fly home for the holiday?
A: Even though in general, planes can be safe, it's not totally safe, just like anywhere when you're out in the environment with people. (You have to consider) whether or not in your family you have a situation where you have elderly people or people who have underlying conditions that would put them at a higher risk of a serious outcome. That should determine what your decision is about the risk you're willing to take. The risk of not traveling is less than the risk of traveling. We don't quantify that. We don't know exactly how much that is. So you've got to decide during this period of a lot of infection going on … do you want to traveland go to a Thanksgiving meal where there may be 12, 15, 20 people?
Q. What is your own family doing this year?
A. I have three adult daughters who live in different parts of the country. They made a decision because of my age that as much as they would love to see me, and my wife and I would love to see them, that they are not going to come for Thanksgiving. So we decided that my wife and I are going to say we had a great Thanksgiving last year and we're looking forward to a great Thanksgiving next year. But (this year) we're going to call a time out.
Q: On Tuesday, you said that the time has come for a less disjointed, more unified national response. Have we passed the point where it makes sense for every city and county and state to be issuing its own guidelines and curfews?
A: There are obviously going to be some differences, because we have such a large, diverse country. But the differences shouldn't be fundamental. There should be really some common denominators that everyone follows. We've got to say, ‘OK, folks, enough is enough with this political divisiveness, with this claiming that people are making things up. Get rid of these ridiculous conspiracy theories and realize this is a public health crisis.’ … We don't want to shut down as a nation because of the psychological and economic consequences of that. But we at least have got to be consistent in doing some fundamental things, so that's what concerns me. We're in a vulnerable position.
Q. How vulnerable?
A. The data speak for themselves. We have over 11 million infections. We have (more than) 250,000 deaths. When you look at the map, where the colors that get darker and redder show that there's increased activity, it's almost the entire country. Things are going in the wrong direction in an arena of increased risk, namely the cooler and colder weather. I mean, let's go, folks. What about that don't you understand?
Q: Do you have a strategy to reach the skeptics? Can they be reached?
A: It's very frustrating and, in many respects, it is beyond frustrating because as a person of science, you're guided by the data. Sometimes the data are not clear. Sometimes you get studies that vary a bit and confuse people. But sometimes data are really solid, and you can't run away from data that's solid.
Q. What about people who claim COVID is no worse than the flu?
A. You have (over 250,000 coronavirus) deaths, 11 million infections and 70,000 people in the hospital. Flu doesn't even come close. When you ask me about frustration, which borders on pain, it’s that either people don't want to look at the data or they look at the data and they say it's fake. No, it isn't fake. … This is a global issue. I tell the people who deny or think that this is nothing, do you mean that every single country in Europe is doing the same thing, is making things up? They're not. I mean, it's so obvious.
Q. How is the latest surge manifesting itself?
A. Go to Billings, Montana, where this intensive care (doctor told NPR that they) have 24 ICU beds, but yesterday we had 44 ICU patients. You never, ever see that with seasonal flu. That's the issue of the day.
Q. Some people are just very resistant to data and facts. Is there really anything that we can do, or does it really depend more on national leadership?
A: What we do need is a consistency of message. … This is real, and if the divisiveness is so severe that people don't think it's real when people are flooding hospitals and dying at a rate that we haven't seen with a disease of this type in 102 years, I hope that's enough of a stimulus for us to drop back as a nation and say, hey, folks, we got to stop talking to each other about what this divide is between us, because it is mind boggling in many respects.
Q: Have there been discussions with the incoming Biden camp about finding better ways to communicate with the public?
A: No, there have not been any formal discussions.
Q: Do you wish that there were discussions?
A: Yes. … I have served under six administrations and have witnessed and been a part of five transitions. Transitions are really important. They are important because you don't want to miss a step. I use the metaphor of a relay race where, when you look at a relay race and someone is running fast and they pass the baton on to the next person in the relay, you don't have the person running stop and then have the next person start from a stop. You're all running together and you pass the baton. That's where the smooth transition is.
Q. Was there a smooth transition in 2016?
A. I can remember four years ago with the transition of the Obama administration to the Trump administration. (There) was a meeting in the Old Executive Office building where I was there talking about the concept of emerging infections and why it would be important to be able to know and understand that they do occur and they occur in a way that sometimes is insidious. I mean, that's what I'm talking about. That kind of thing makes it easier to just go from one to the other. So, yes, I would wish that we would be able to do that. That would be helpful.
Q: If Ron Klain, Biden's incoming chief of staff who has a lot of experience with public health, were to call you after this meeting, are you allowed to take his call? Or have you been told you're forbidden to speak with the Biden transition team?
A: I have not been formally told that anything is forbidden. But it's quite obvious that this is a very sensitive period. … I have tried to the best of my ability to stay out of the political aspects and just focus on my role as a public health person, a physician and a scientist. To be honest with you, I believe that the Biden people, including Ron Klain, understand that and don't want to put me in a compromised position.
Q: New York and several other states are saying they want an extra layer of review for any vaccines that are approved by the Food and Drug Administration, essentially because they don't trust anything coming out of the Trump administration. Is that extra layer of review either wise or appropriate?
A: I understand what they're doing, (but) I think they may have the unintended consequence of creating a layer of doubt about the ultimate decision and recommendation that a vaccine is safe and effective. And maybe by my saying this here, I can have a public outreach to them to explain that the process of a decision, whether something is safe and effective, is really an independent process.
Q. What is the process?
A. The data and safety monitoring board is beholden to no one, not to the administration, not to the company and not to me. They're independent, and they independently and intermittently look at the data. And the last time they looked at the data, this independent group said the data are extraordinary. There were 95 cases (of COVID-19) — 90 in the placebo group and five in the vaccine group, which was a 94.5% efficacy. There were 11 severe cases — zero in the vaccine group, 11 in the placebo group. They examined that data carefully. The data were then presented to me, which they did this past Sunday afternoon.
Q. What happens next?
A. The data will be presented to the FDA to get an emergency use authorization. The career scientists, who are beholden to no one, will look at the data and then they will get advice from their advisory board, which is called the Vaccines and Related Biological Products Advisory Committee. That group will then advise the FDA as to whether or not they should approve the vaccine for an EUA or for a biological license application. Then those data will be published and will be public for all the scientists around to look at. It is transparent, and it's independent.
Q. Can you understand why some people are skeptical?
A. I know there's a lot of stuff coming out of Washington to get people concerned. Is there pressure, or what have you? But I can tell you that the process is such that I would — when it gets approved by the FDA, given the time of my turn, when it comes — take the vaccine and I would recommend that my family take the vaccine.
Q: If the first doses of vaccine are available for front-line workers in December and January, when should the U.S. general population expect to get theirs?
A: Just the normal everyday person in the street, likely starting sometime in April as we go into May, June, July. So that hopefully, by the time we get to the end of the second quarter and looking at the third quarter, if we do get people vaccinated to a high degree, then you can start talking about this umbrella or blanket of protection on society that would diminish dramatically the risk of a person being exposed or even being infected.
Q. And when would life return to normal?
A. When so many people are protected, that's when you get into the real herd immunity, namely, the overwhelming majority of the population is protected because of the vaccine. So that's why when people ask when do I think when they get back to some sort of normality, it's kind of dependent upon us. One other comment that I want to link to my answer, is that just because you're vaccinated does not mean that you should abandon all public health measures. The vaccine is a complement, not a substitute. It would be a substitute when you get everybody vaccinated and there's no virus around, sort of like with measles.
Q: A survey that came out in September said that only 32% of Black Americans said that they would trust the vaccine enough to take it. How would you reach out to the Black community and reassure people that taking the vaccine is actually safe?
A: Well, the first thing is that we need to understand the truly understandable reasons why minority communities, particularly African Americans, feel that way. Because history of the interaction between the federal government and the arena of health is not a good history dating back to the Tuskegee issues and even others that have followed. … So there are two things. One, show transparency and consistency and independence. And two, outreach to the community by people who are trusted by the community.
Q. Were minority groups adequately represented in the clinical trials for the Moderna vaccine developed in collaboration with the National Institutes of Health?
A. Here at NIH (we worked) very hard to get minority representation in the actual clinical trial. So that when the clinical trial is proven to be safe and effective, you can go to the brown and Black community and say, you know, you all participated in the trial and we know it works and is safe in you because here's the data from the trial. What you don't want to do is to get a ‘white man's vaccine’ and say we're going to give it to Black people, or say that it's not been properly tested in an equitable way in brown and Black people. So what we did with the trial is we said we want representation of the elderly, white, brown, Black, people with underlying conditions so that we can get a feel if it's effective across the board.
Q: And then you need to persuade people to take it.
A: That's really important. We know we have an efficacious vaccine. We've proven it. It's 94.5%-95% efficacious. It would not be effective if people don't take it. If you have 30%, 40%, 50% of the population that don't want to take it, you have an efficacious vaccine that is being blocked from being effective because people aren't taking it. The best case scenario, if we really want to crush this outbreak, is to have a highly efficacious vaccine, which we already know we have. We have two of them, and we likely will have more than two. And to make that vaccine effective by having the overwhelming majority of the population take it. It would be extremely detrimental if we have an efficacious vaccine and people don't take it. It would be actually a tragedy.
Q: Once you get the vaccine, how long does it take to develop immunity?
A: You can expect that about seven days or so following the second boost, you can actually get a considerable degree of protection. In fact, some people might even get a degree of protection after the first dose, maybe two weeks or three weeks after the first dose. But clearly, when you get out to about seven days after the second dose, you can be fairly certain that you were in a good degree of immunity.
Q. How long will that immunity last?
A. We do not know that. That's an important question. And that's the reason why these studies go out for two years.
Q: At what point does it become unethical to keep people in the placebo groups?
A: It becomes unethical if you have widespread availability of the vaccine that's highly effective and just for the purpose of the study, you're keeping them in a placebo group. But you can extend it for a week or two to get data to really nail down what you're dealing with, because the long-range benefit to the individual and to society would likely be much, much greater for that extra week or two that you keep them on.
Q. If multiple vaccines are available, how do I know which one to take?
A. The availability of the distribution is going to be recommended to the CDC (Centers for Disease Control and Prevention), which is the final decider as to what the prioritization is. … You're going to see kind of a graded rollout of vaccines. What you might find, which we've seen with other vaccines, is that some might be more appropriate for the elderly versus the young, some maybe more for pregnant women versus people with underlying conditions. We don't know that yet. … What we're hearing in the preliminary analysis of the data is that (the first two vaccines appear) tobe effective across all the subgroups, which is really quite good news.
Q: What concerns you most right now?
A: If you go into the winter or the late fall and the (daily) baseline of infections is over 100,000, it becomes so difficult (to control surges) because the degree of community spread that represents is really profound. And it makes what we have to do so much more difficult. Which is the reason why I get back to what I said — please folks, hang on to the extent that we can, because help is on the way with a vaccine. This is not going to be an indefinite situation. It will change, and it will end.
This Interview was originally published on USA Today.
